I. Overview
-Antimicrobial therapy takes advantage of the biochemical differences that exist between microorganisms and human beings.
-Antimicrobial drugs are effective in the treatment of infections because of their selective toxicity; that is, they have the ability to injure or kill an invading microorganism without harming the cells of the host.
-In most instances, the selective toxicity is relative rather than absolute, requiring that the concentration of the drug be carefully controlled to attack the microorganism while still being tolerated by the host.
II. Selection of Antimicrobial Agents
Selection of the most appropriate antimicrobial agent requires knowledge of:
1) the organism's identity,
2) the organism's susceptibility to a particular agent,
3) the site of the infection,
4) patient factors,
5) the safety of the agent, and
6) the cost of therapy.
II. Selection of Antimicrobial Agents
However, some critically ill patients require empiric therapy- that is, immediate administration of drug(s) prior to bacterial identification and susceptibility testing.
A. Identification of the infecting organism
-Characterization of the organism is central to selection of the proper drug.
Cultivation and identification
-It is generally necessary to culture the infective organism to arrive at a conclusive diagnosis and to determine the susceptibility of the bacteria to antimicrobial agents.
Gram stain
A rapid assessment of the nature of the pathogen
Useful in identifying the presence and morphologic features of microorganisms
Body fluids that are normally sterile (cerebrospinal fluid [CSF], pleural fluid, synovial fluid, peritoneal fluid, and urine) are used
Definite identification (Others)
Definitive identification of the infecting organism may require other laboratory techniques, such as detection of microbial antigens, microbial DNA or RNA, or detection of an inflammatory or host immune response to the microorganism.
B. Empiric therapy prior to identification of the organism
Ideally, the antimicrobial agent used to treat an infection is selected after the organism has been identified and its drug susceptibility established.
However, in the critically ill patient, such a delay could prove fatal, and immediate empiric therapy is indicated.
1. Timing
Acutely ill patients with infections of unknown origin require immediate treatment.
A neutropenic patient (one who has a reduction in neutrophils, predisposing the patient to infections),
A patient with severe headache, a rigid neck, and sensitivity to bright lights (symptoms characteristic of meningitis)
2. Selecting a drug
The choice of drug in the absence of susceptibility data is influenced by the site of infection and the patient's history (for example, whether the infection was hospital- or community-acquired, whether the patient is immunocompromised, as well as the patient's travel record and age).
C. Determination of antimicrobial susceptibility
After a pathogen is cultured, its susceptibility to specific antibiotics serves as a guide in choosing antimicrobial therapy.
Some pathogens usually have predictable susceptibility patterns to certain antibiotics.
Such as Streptococcus pyogenes and Neisseria meningitidis
In contrast, some species often show unpredictable susceptibility patterns to various antibiotics and require susceptibility testing to determine appropriate antimicrobial therapy.
Such as most gram-negative bacilli, enterococci, and staphylococcal species
1. Bacteriostatic vs. bactericidal drugs
Bacteriostatic drugs arrest the growth and replication of bacteria
The body's immune system attacks, immobilizes, and eliminates the pathogens.
If the drug is removed before the immune system has scavenged the organisms, enough viable organisms may remain to begin a second cycle of infection.
Bactericidal drugs kill bacteria
Because of their more aggressive antimicrobial action, these agents are often the drugs of choice in seriously ill patients.
D. Effect of the site of infection on therapy: The blood-brain barrier
Adequate levels of an antibiotic must reach the site of infection for the invading microorganisms to be effectively eradicated.
Capillaries with varying degrees of permeability carry drugs to the body tissues.
Capillary in brain: formed by the single layer of tile-like endothelial cells fused by tight junctions.
The penetration and concentration of an antibacterial agent in the CSF is particularly influenced by the following:
Lipid solubility of the drug:
The lipid solubility of a drug is a major determinant of its ability to penetrate into the brain.
For example, lipid-soluble drugs, such as the quinolones and metronidazole, have significant penetration into the CNS.
In contrast, β-lactam antibiotics, such as penicillin, are ionized at physiologic pH and have low solubility in lipids. They therefore have limited penetration through the intact blood-brain barrier under normal circumstances.

In infections such as meningitis, in which the brain becomes inflamed, the barrier does not function effectively, and local permeability is increased.
Some β-lactam antibiotics can then enter the CSF in therapeutic amounts.
Molecular weight of the drug:
A compound with a low molecular weight has an enhanced ability to cross the blood-brain barrier, whereas compounds with a high molecular weight (for example, vancomycin) penetrate poorly, even in the presence of meningeal inflammation.
Protein binding of the drug:
A high degree of protein binding of a drug in the serum restricts its entry into the CSF. Therefore, the amount of free (unbound) drug in serum, rather than the total amount of drug present, is important for CSF penetration.
D. Patient factors
-Immune system
-Renal dysfunction
-Hepatic dysfunction
-Poor perfusion
-Age
-Pregnancy
-Lactation
E. Safety of the agent
Penicillins: The least toxic of all drugs, because they interfere with a site unique to the growth of microorganisms.
Chloramphenicol: Less microorganism specific and are reserved for life-threatening infections because of the drug's potential for serious toxicity to the patient.
Article Posted By: Md. Enamul Hoque Khan
Student of MPharm. Department of Pharmacy,
East West University
-Antimicrobial therapy takes advantage of the biochemical differences that exist between microorganisms and human beings.
-Antimicrobial drugs are effective in the treatment of infections because of their selective toxicity; that is, they have the ability to injure or kill an invading microorganism without harming the cells of the host.
-In most instances, the selective toxicity is relative rather than absolute, requiring that the concentration of the drug be carefully controlled to attack the microorganism while still being tolerated by the host.
II. Selection of Antimicrobial Agents
Selection of the most appropriate antimicrobial agent requires knowledge of:
1) the organism's identity,
2) the organism's susceptibility to a particular agent,
3) the site of the infection,
4) patient factors,
5) the safety of the agent, and
6) the cost of therapy.
II. Selection of Antimicrobial Agents
However, some critically ill patients require empiric therapy- that is, immediate administration of drug(s) prior to bacterial identification and susceptibility testing.
A. Identification of the infecting organism
-Characterization of the organism is central to selection of the proper drug.
Cultivation and identification
-It is generally necessary to culture the infective organism to arrive at a conclusive diagnosis and to determine the susceptibility of the bacteria to antimicrobial agents.
Gram stain
A rapid assessment of the nature of the pathogen
Useful in identifying the presence and morphologic features of microorganisms
Body fluids that are normally sterile (cerebrospinal fluid [CSF], pleural fluid, synovial fluid, peritoneal fluid, and urine) are used
Definite identification (Others)
Definitive identification of the infecting organism may require other laboratory techniques, such as detection of microbial antigens, microbial DNA or RNA, or detection of an inflammatory or host immune response to the microorganism.
 |
| Figure: Some laboratory techniques that are useful in the diagnosis of microbial diseases |
B. Empiric therapy prior to identification of the organism
Ideally, the antimicrobial agent used to treat an infection is selected after the organism has been identified and its drug susceptibility established.
However, in the critically ill patient, such a delay could prove fatal, and immediate empiric therapy is indicated.
1. Timing
Acutely ill patients with infections of unknown origin require immediate treatment.
A neutropenic patient (one who has a reduction in neutrophils, predisposing the patient to infections),
A patient with severe headache, a rigid neck, and sensitivity to bright lights (symptoms characteristic of meningitis)
2. Selecting a drug
The choice of drug in the absence of susceptibility data is influenced by the site of infection and the patient's history (for example, whether the infection was hospital- or community-acquired, whether the patient is immunocompromised, as well as the patient's travel record and age).
C. Determination of antimicrobial susceptibility
After a pathogen is cultured, its susceptibility to specific antibiotics serves as a guide in choosing antimicrobial therapy.
Some pathogens usually have predictable susceptibility patterns to certain antibiotics.
Such as Streptococcus pyogenes and Neisseria meningitidis
In contrast, some species often show unpredictable susceptibility patterns to various antibiotics and require susceptibility testing to determine appropriate antimicrobial therapy.
Such as most gram-negative bacilli, enterococci, and staphylococcal species
1. Bacteriostatic vs. bactericidal drugs
Bacteriostatic drugs arrest the growth and replication of bacteria
The body's immune system attacks, immobilizes, and eliminates the pathogens.
If the drug is removed before the immune system has scavenged the organisms, enough viable organisms may remain to begin a second cycle of infection.
Bactericidal drugs kill bacteria
Because of their more aggressive antimicrobial action, these agents are often the drugs of choice in seriously ill patients.
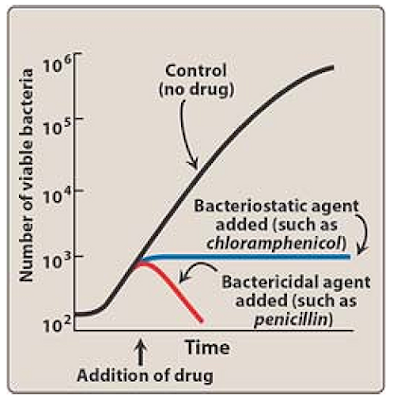 |
| Figure Effects of bactericidal and bacteriostatic drugs on the growth of bacteria in vitro. |
2. Minimum inhibitory concentration
To determine the minimum inhibitory concentration (MIC), tubes containing serial dilutions of an antibiotic are inoculated with the organism whose susceptibility is to be tested.
The tubes are incubated and later observed to determine the MIC- that is, the lowest concentration of antibiotic that inhibits bacterial growth. (FIG)
To provide effective antimicrobial therapy, the clinically obtainable antibiotic concentration in body fluids should be greater than the MIC.
3. Minimum bactericidal concentration
This quantitative assay determines the minimum concentration of antibiotic that kills the bacteria under investigation.
The tubes that show no growth in the MIC assay are subcultured into antibiotic-free agar media.
The minimum bactericidal concentration is the lowest concentration of antimicrobial agent that results in a 99.9 percent decline in colony count after overnight broth dilution incubations.
Antimicrobials are usually regarded as bactericidal if the MBC is no more than four times the MIC.
To determine the minimum inhibitory concentration (MIC), tubes containing serial dilutions of an antibiotic are inoculated with the organism whose susceptibility is to be tested.
The tubes are incubated and later observed to determine the MIC- that is, the lowest concentration of antibiotic that inhibits bacterial growth. (FIG)
To provide effective antimicrobial therapy, the clinically obtainable antibiotic concentration in body fluids should be greater than the MIC.
3. Minimum bactericidal concentration
This quantitative assay determines the minimum concentration of antibiotic that kills the bacteria under investigation.
The tubes that show no growth in the MIC assay are subcultured into antibiotic-free agar media.
The minimum bactericidal concentration is the lowest concentration of antimicrobial agent that results in a 99.9 percent decline in colony count after overnight broth dilution incubations.
Antimicrobials are usually regarded as bactericidal if the MBC is no more than four times the MIC.

D. Effect of the site of infection on therapy: The blood-brain barrier
Adequate levels of an antibiotic must reach the site of infection for the invading microorganisms to be effectively eradicated.
Capillaries with varying degrees of permeability carry drugs to the body tissues.
Capillary in brain: formed by the single layer of tile-like endothelial cells fused by tight junctions.
The penetration and concentration of an antibacterial agent in the CSF is particularly influenced by the following:
Lipid solubility of the drug:
The lipid solubility of a drug is a major determinant of its ability to penetrate into the brain.
For example, lipid-soluble drugs, such as the quinolones and metronidazole, have significant penetration into the CNS.
In contrast, β-lactam antibiotics, such as penicillin, are ionized at physiologic pH and have low solubility in lipids. They therefore have limited penetration through the intact blood-brain barrier under normal circumstances.

In infections such as meningitis, in which the brain becomes inflamed, the barrier does not function effectively, and local permeability is increased.
Some β-lactam antibiotics can then enter the CSF in therapeutic amounts.
Molecular weight of the drug:
A compound with a low molecular weight has an enhanced ability to cross the blood-brain barrier, whereas compounds with a high molecular weight (for example, vancomycin) penetrate poorly, even in the presence of meningeal inflammation.
Protein binding of the drug:
A high degree of protein binding of a drug in the serum restricts its entry into the CSF. Therefore, the amount of free (unbound) drug in serum, rather than the total amount of drug present, is important for CSF penetration.
 |
| Figure Effects of bactericidal and bacteriostatic drugs on the growth of bacteria in vitro. |
D. Patient factors
-Immune system
-Renal dysfunction
-Hepatic dysfunction
-Poor perfusion
-Age
-Pregnancy
-Lactation
E. Safety of the agent
Penicillins: The least toxic of all drugs, because they interfere with a site unique to the growth of microorganisms.
Chloramphenicol: Less microorganism specific and are reserved for life-threatening infections because of the drug's potential for serious toxicity to the patient.
Article Posted By: Md. Enamul Hoque Khan
Student of MPharm. Department of Pharmacy,
East West University




 Wednesday, August 28, 2013
Wednesday, August 28, 2013
 Ask2Pharma
Ask2Pharma



 Posted in:
Posted in: 




0 comments:
Post a Comment